Peptides, PCOS & Weight Loss: What to Know Before You Try Them

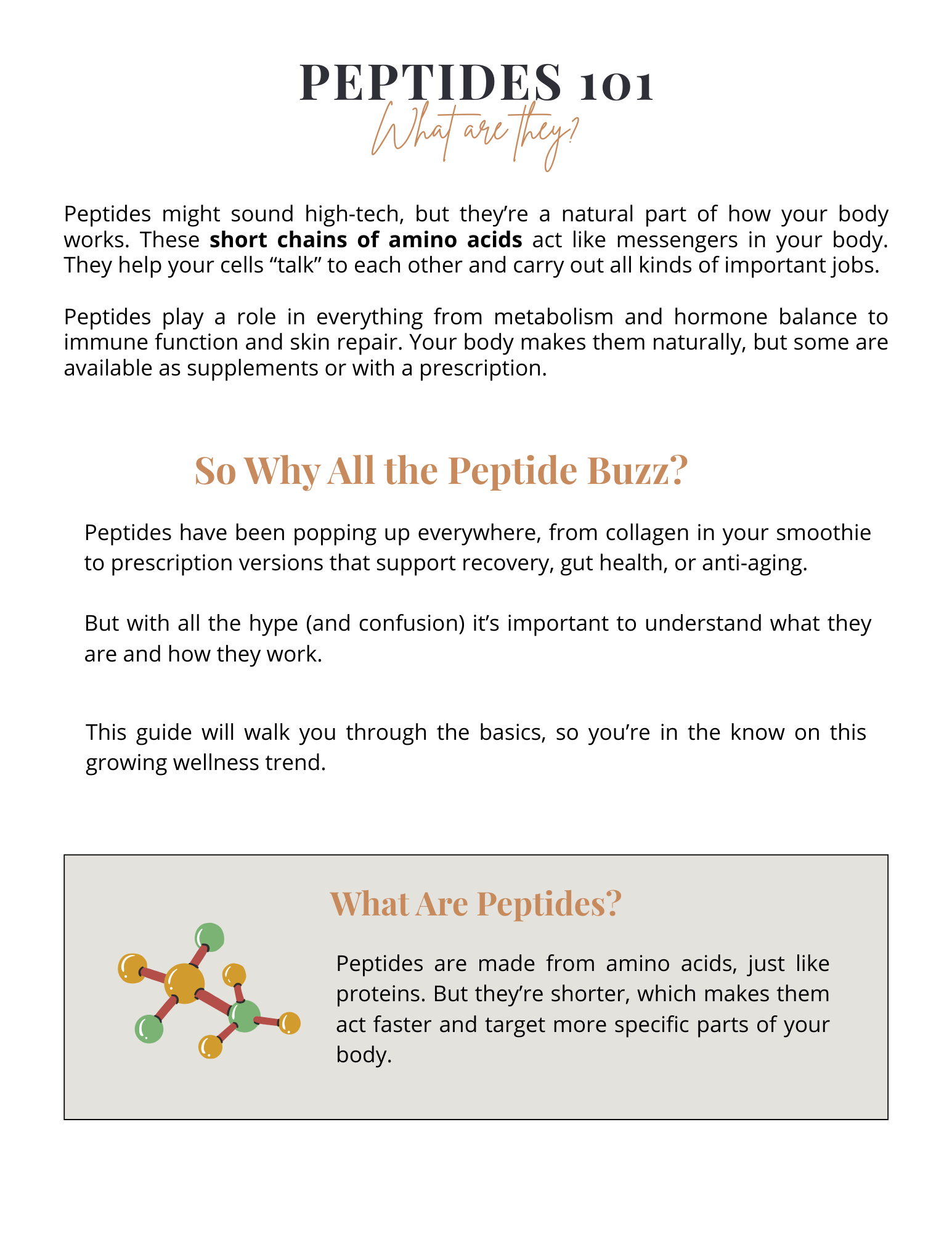
Peptides are trending right now. From weight loss to hormone health to anti-aging claims, they’re being positioned as the next big solution for almost everything.
And for women with PCOS, that can feel both exciting and overwhelming.
PCOS already comes with enough noise. Conflicting advice. Trend-driven “fixes.” And the constant pressure to find the thing that will finally make weight loss easier, hormones calmer, or energy come back.
This guide isn’t about selling peptides as a miracle solution or warning you away from them entirely. It’s about understanding where they might fit, where they don’t, and why your nutrition & exercise foundation still matters more than anything else.
One reason peptides get so much attention in PCOS and weight loss is because they work at the signaling level.
PCOS isn’t just a calorie problem. It’s a communication problem.
Hormones, blood sugar, appetite cues, inflammation, stress responses. When those signals are dysregulated, fat loss becomes harder no matter how “perfect” your diet looks on paper.
That’s why peptides sound appealing. They’re often described as targeted, precise, and efficient. And in some cases, they can influence systems that are commonly disrupted in PCOS.
But here’s the key point that often gets skipped:
Peptides don’t replace foundational health. They layer on top of it.
If blood sugar is unstable, sleep is poor, stress is chronically high, and nutrition is inconsistent, no peptide will override that long-term.
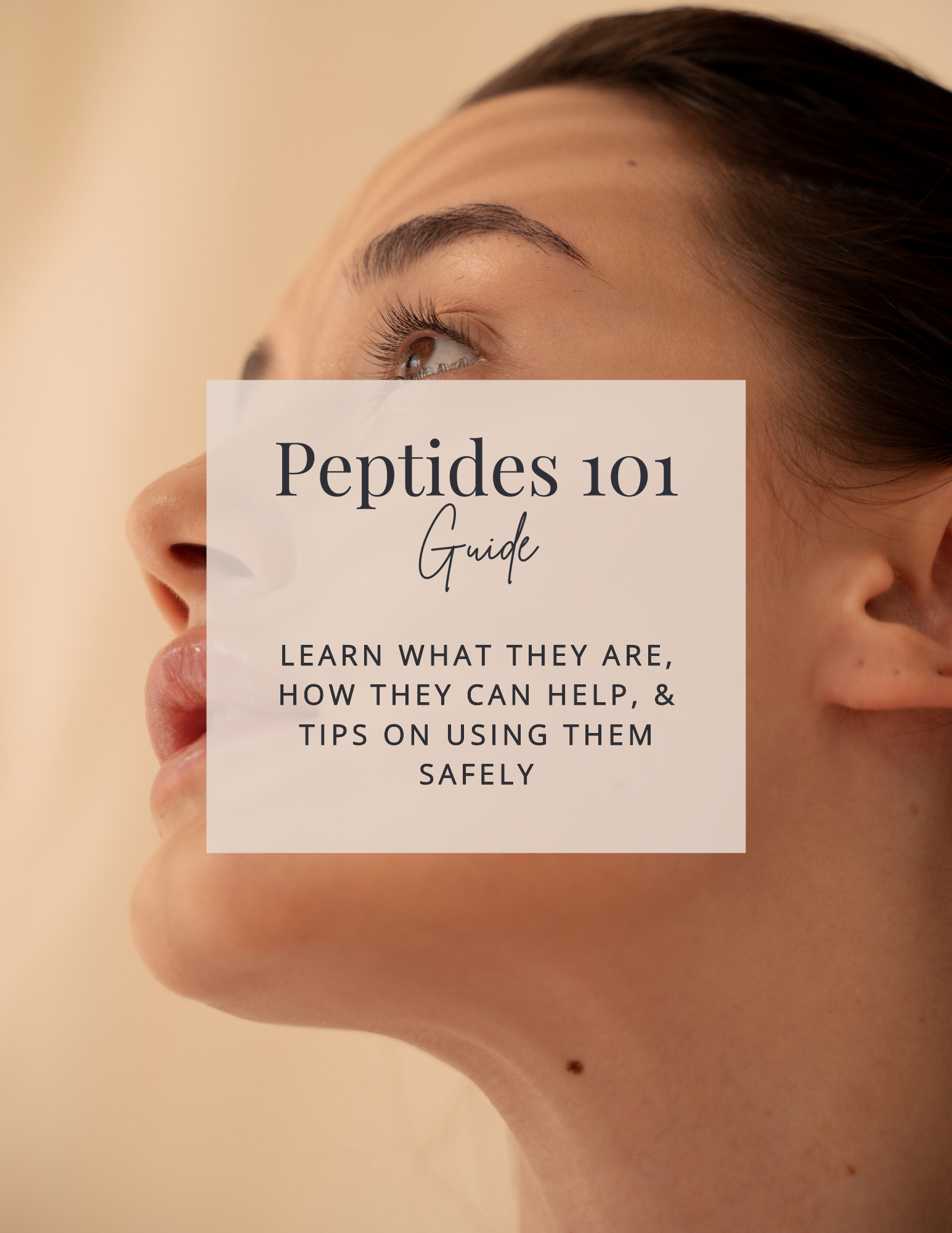
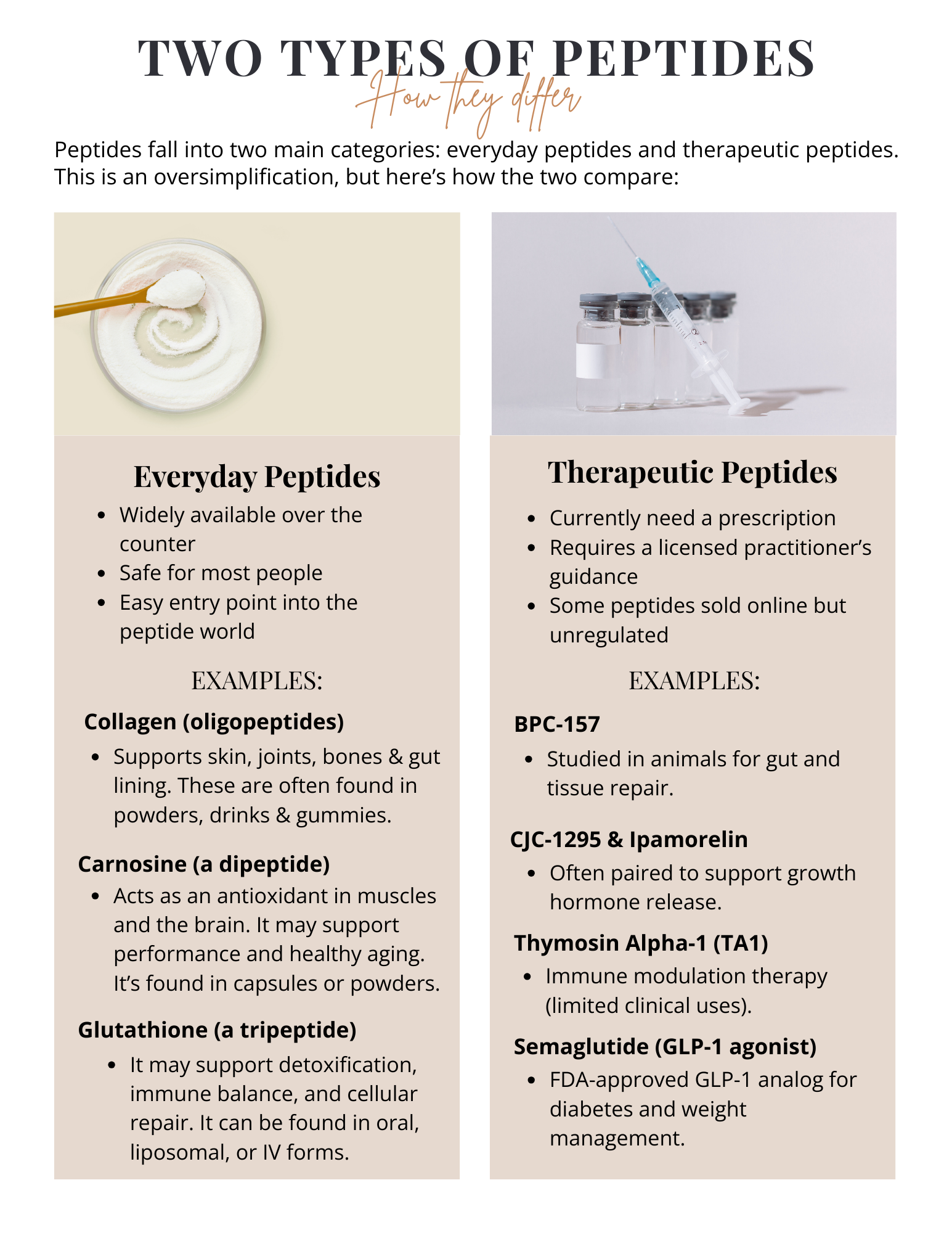
Two Types of Peptides
This distinction matters a lot for women with PCOS.
Many people hear the word “peptides” and lump collagen in their coffee and injectable weight loss drugs into the same category. They’re not the same thing. They don’t act the same way, and they don’t carry the same level of responsibility or risk.
For PCOS specifically, this matters because:
-
Weight loss resistance can push people toward more aggressive interventions too early
-
Hormone-sensitive conditions require more caution, not less
-
“Just because it’s popular” is not a great decision making framework
Understanding whether something is a basic nutritional support or a medical intervention helps you decide when it’s appropriate to even consider it.
Why Peptides Are Popular
Peptides are often marketed as shortcuts, but what they really are are amplifiers.
They may amplify recovery.
They may amplify appetite suppression.
They may amplify metabolic signals.
They may amplify immune or inflammatory responses.
And amplification can be helpful or problematic depending on the context.
For women with PCOS, this is especially important because many already live in a state of physiological overdrive. Elevated insulin. Elevated cortisol. Chronic inflammation. Pushing the gas pedal harder isn’t always the answer.
Sometimes the work is actually about slowing down, stabilizing, nourishing, and rebuilding trust with your body before adding anything that increases intensity.
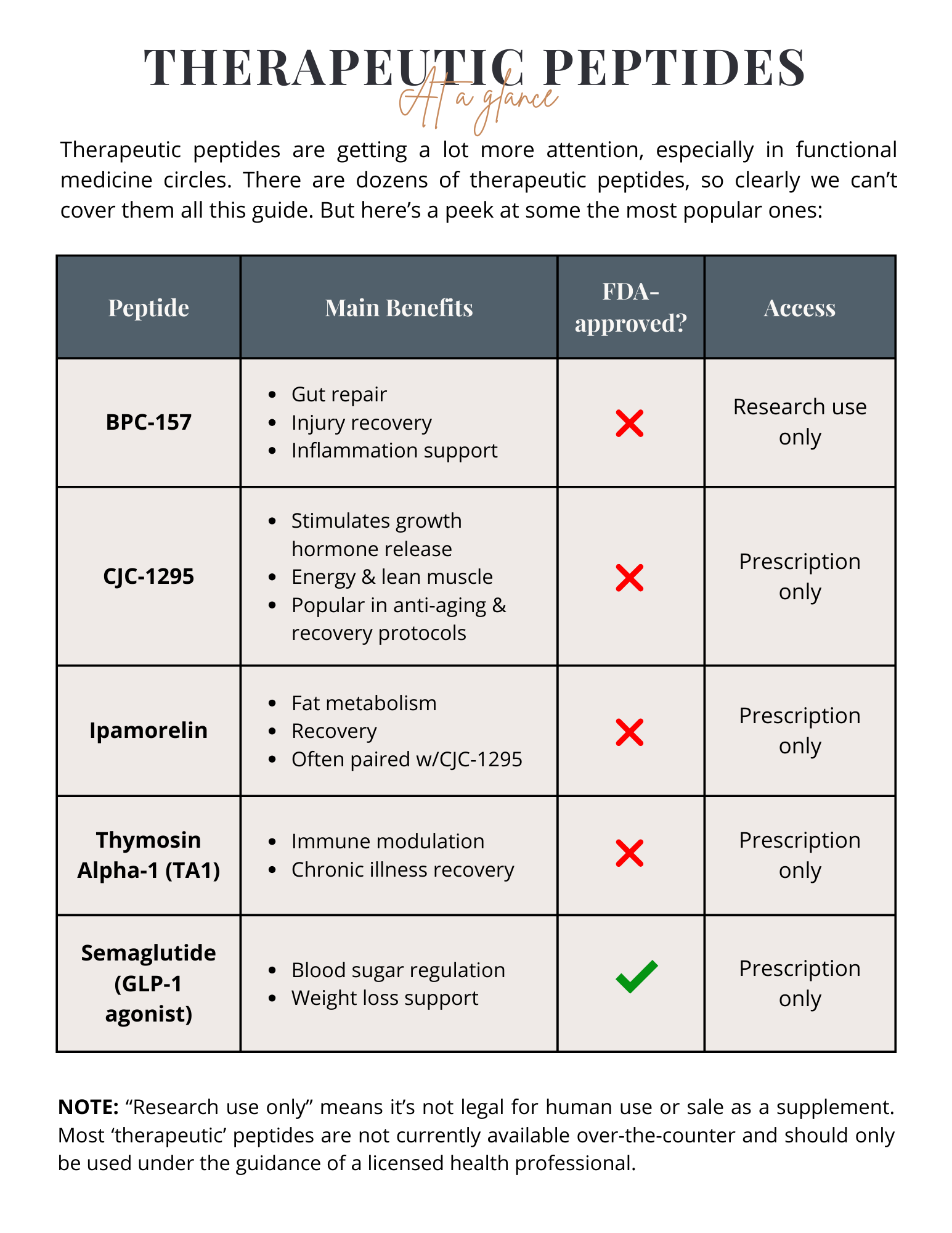
Therapeutic Peptides: At a Glance
This is where nuance matters.
Some peptides are FDA-approved. Some aren’t. Some are prescription-only. Some are sold online under labels that exist in legal gray areas.
But here’s the honest truth that often gets lost in internet debates:
FDA-approved does not automatically mean “best.”
Not FDA-approved does not automatically mean “dangerous.”
Approval status tells you about regulatory pathways, not whether something is appropriate for you, at this time, in your body, with your history.
This is why independent thinking, practitioner guidance, and personal context matter more than headlines or trends.
And before anything else, making sure you've built your foundation on proper eating and consistent exercise is crucial. Start here, then consider peptides.
Therapeutic Peptides: A Closer Look
In PCOS conversations, therapeutic peptides often enter the picture because:
-
Weight loss feels impossible despite effort
-
Hunger feels dysregulated
-
Muscle loss is a concern during dieting
-
Inflammation or injury limits exercise capacity
These are real struggles. And it’s valid to explore options.
But it’s also important to ask better questions:
-
What problem am I actually trying to solve?
-
Is this addressing a root cause or managing a symptom?
-
Have I built the foundation that makes this safer and more effective?
Peptides may have a place for some people. They’re not a prerequisite for progress.
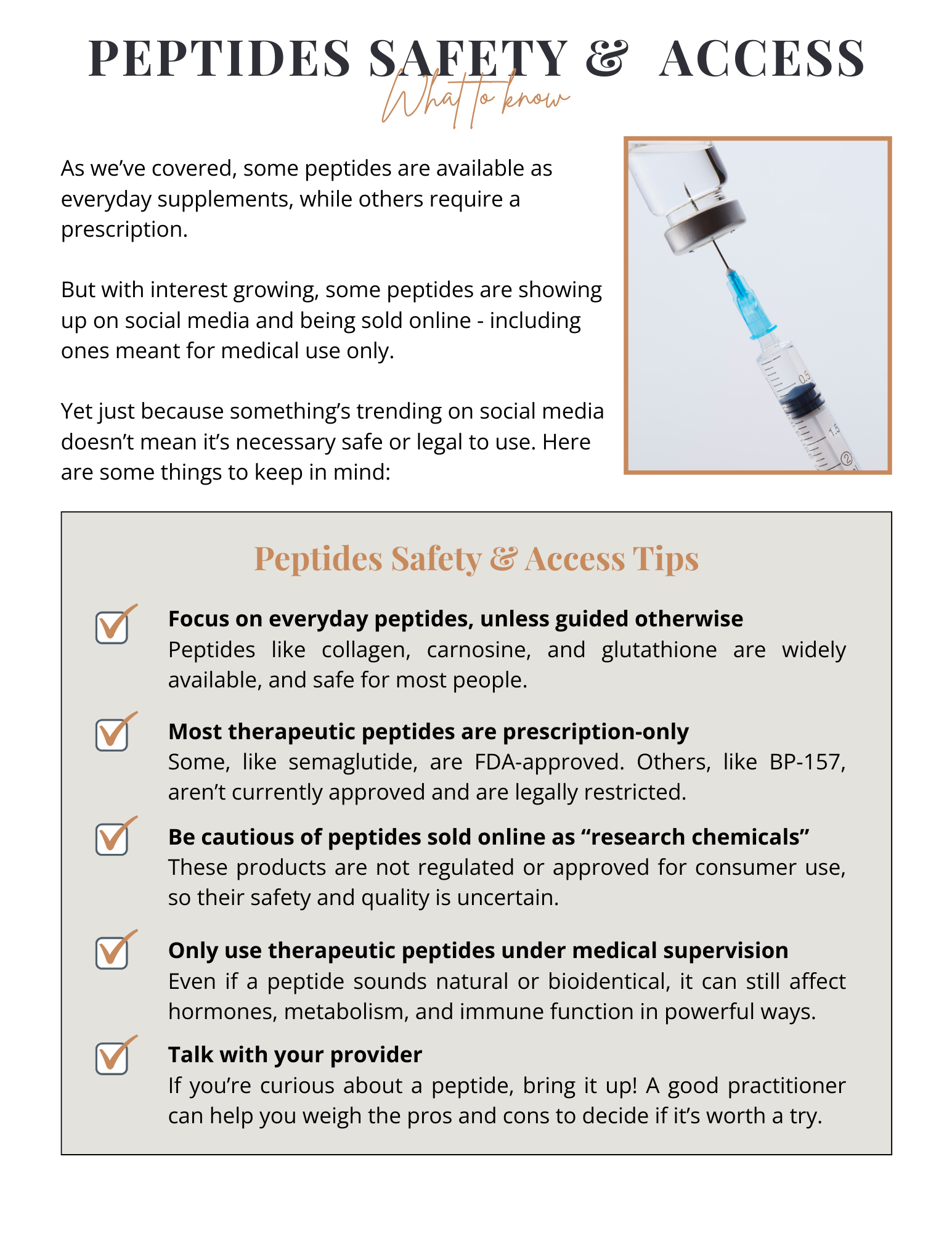
Peptides Safety & Access
This is where social media does the most damage.
Just because something is trending doesn’t mean it’s well understood. And just because something is labeled “natural” or “bioidentical” doesn’t mean it’s harmless.
For women with PCOS, hormone-sensitive pathways deserve respect. Anything that alters appetite, insulin signaling, stress hormones, or immune function should be approached thoughtfully.
Curiosity is healthy. Blind trust is not.
Doing your own research doesn’t mean going down internet rabbit holes. It means:
-
Understanding mechanisms, not just outcomes
-
Knowing what data exists and what doesn’t
-
Being honest about your readiness for intervention
OTC vs. Therapeutic Peptides
Here’s the part I care about most.
If you don’t have:
-
Consistent, blood-sugar-supportive nutrition
-
Adequate protein intake
-
Strength training and regular movement
-
Stress management and sleep support
Then peptides are not the missing piece.
Those fundamentals are hormone therapy.
They are metabolic medicine.
They are the reason anything else works better.
And the irony is, many women with PCOS find that once those foundations are in place, they no longer need the aggressive tools they once thought they did.
And if they do choose to use peptides later?
Their body is far better prepared to respond well.